Recent Posts
Reshaping your future: Exploring reconstruction options after breast cancer

A cancer journey is full of decisions. This may include where to receive treatment, the type of treatment you want, if you should participate in a clinical trial, if you should seek a second opinion and if reconstructive surgery is right for you.
It's common to experience a wide range of emotions over these decisions. After your cancer diagnosis, you may feel anxious, afraid, angry or overwhelmed, and wonder how you can cope during the days ahead. These are expected feelings.
One decision that can feel overwhelming and cause stress and anxiety is how your appearance may change after treatment. Mastectomy, lumpectomy and radiation can drastically change a person's appearance and body contour. While some people decide that breast tissue reconstruction is unnecessary after treatment, others wish to restore their breasts if possible.
Many reconstruction options are available to give breasts a more natural appearance after cancer treatment. Talk with your healthcare team about your desires and which option may be best for you.
Here are the most common breast reconstruction techniques.
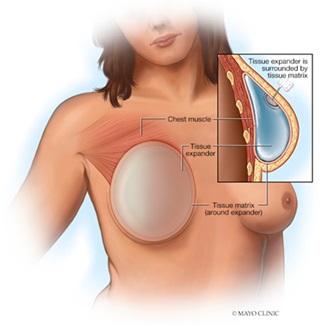
Tissue expansion and implant
During tissue expansion, an expandable, balloon-like implant is inserted in the place of the breast, either above or under your chest muscle. This temporary implant is gradually filled with saline over several weeks or months. This can be done at the time of your mastectomy or at a later time. The tissue expander is gradually inflated to stretch the skin and tissue over your chest and make room for a permanent implant.
After the tissue is adequately expanded, your surgeon performs a second surgery to remove the tissue expander and replace it with a permanent implant. This can be a silicone or saline device that reshapes your breast and is filled with silicone gel or salt water.
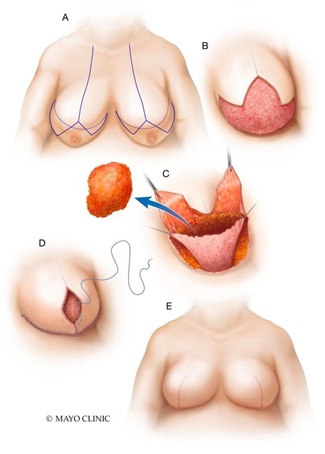
Flap procedure
Breast reconstruction with flap surgery involves taking a section of tissue from one area of your body and relocating it to create a new breast mound. Most of the time, this is done as a separate procedure from your mastectomy.
Breast reconstruction with flap surgery is the most complex breast reconstructive option. Your surgeon transfers a section of skin, muscle, fat and blood vessels from another part of your body to your chest to create a new breast mound. In some cases, the skin and tissue need to be augmented with a breast implant or other surgery to achieve the desired breast size.
The tissue for reconstructing your breast most often comes from your abdomen; it may also come from your back or, less commonly, your buttocks.
The most common flap procedures are:
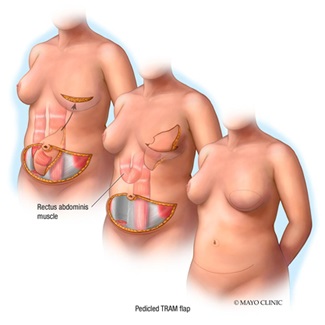
Pedicle TRAM flap
In a pedicle TRAM flap procedure, the surgeon cuts a section of skin, muscle, fat and blood vessels from your abdomen, tunnels the tissue underneath your skin to its new location and uses it to form a new breast mound.
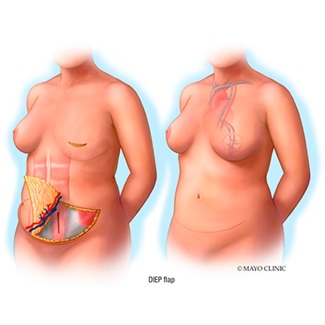
Deep inferior epigastric perforation (DIEP) flap
A newer procedure, DIEP flap, is similar to a TRAM flap, but only skin and fat are removed. Most of the abdominal muscle is left in place, and minimal muscle tissue is taken to form the new breast mound. An advantage to this type of breast reconstruction is that you'll retain more strength in your abdomen.
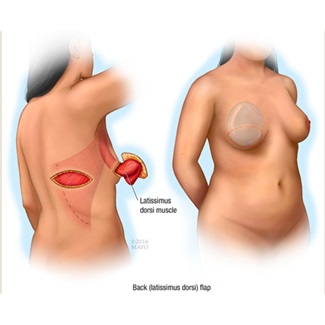
Latissimus dorsi flap
In this flap procedure, the surgeon takes tissue from the latissimus dorsi muscle with skin from your back, tunnels it underneath your arm to its new location and uses it to form a new breast mound.
Goldilocks
The Goldilocks procedure is performed after a mastectomy that removes unhealthy breast tissue. Then the remaining fatty tissue and skin are formed into a breast mound that gives some shape and definition to the breast. This procedure does not produce a large breast mound but does give shape and definition to the breast that can be augmented later if desired.
It's called Goldilocks because it represents a middle-of-the-road option between mastectomy with a flat-chest appearance and full reconstruction with implants, expanders or a flap procedure. The operation is typically used in patients with larger and heavier breasts, but it can be used in some patients with smaller breasts.
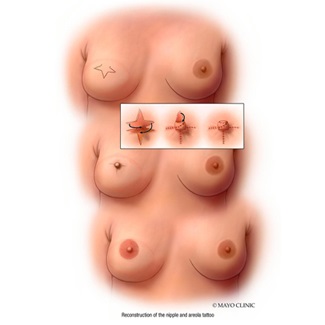
Nipple reconstruction
If you choose, breast reconstruction may also involve reconstruction of your nipple, including 3D tattooing to define the dark area of skin surrounding your nipple called the areola.
Breast reconstruction won't recreate the exact look and feel of your natural breast. However, the contour of your new breast may restore a silhouette similar to what you had before mastectomy. While it may not have the same appearance or feel as your natural breast, it does provide a sense of wholeness after undergoing mastectomy for cancer treatment. Discuss your options and preferences with your healthcare team.
Matthew Sherrill, M.D., is a plastic and reconstructive surgeon in La Crosse, Wisconsin.




